Make It Stop!! Vent Alarms and What to Do with Dr. Andrew Phillips
May 16, 2023
Vent management is a integral skill for the Emergency Medicine doctor, but it is a tricky art. We sat down with Dr. Andrew Phillips, EM and Critical Care trained physician and founder and Editor in Chief of EMCoach, an AI powered board review suite to talk about vent alarms- what they mean, and what to do about them.

Make It Stop!!- Vent Alarms and What To Do with Dr. Andrew Phillips – The SimKit Podcast
Transcript
Jason Hine: Hello, everybody, and welcome back to the SimKit podcast. Today, we’re gonna be talking about vents, vent alarms and I am joined by Dr. Andrew Phillips. Andrew is an ED and critical care physician. He’s the founding medical director for his hospital’s ECMO program. Nice work there. He’s an associate medical director for the ICUs, and is a staff physician for an ED at an affiliate rural hospital, as well. So sometime in the tertiary care ICUs as well as in the rural ED environment. He’s also the founder and editor in chief of EM Coach, a very popular board review suite. So Andrew, thank you so much for joining us on SimKit.
Andrew Phillips: Pleasure to be here. Thank you for the invitation.
Jason Hine: Yeah. So Dr, Phillips vent alarms, and how to manage them. It’s really an integral skill for the ED physician. But I’d say that we’re probably not really all that good at it. So hypothetically say you’re a doc in a remote access hospital and all ICU patients have to be transferred out. You have to know what you. Yeah. Right me as well…
Andrew Phillips: Easy to imagine that, that’s me. 100%.
Jason Hine: Me as well, part of my work. Yeah, I actually, you know, I don’t work in the ICUs but I work all the way from an academic center to a freestanding ER, so very poignant case scenario there, right? But if you’re working in that environment, you have to know what you’re doing when that thing starts beeping at you, but it’s not just the rural community docs, that have to know this say, you work in the Ivory Tower, the academic medical center at the tertiary care hospital. it’s Conference Day. The third year resident, who is fresh off of medical ICU is not there to help you with your vent. That clinician also has to know what they are doing. So Andrew. Why is this skill so important and why are we seemingly so bad at it?
Andrew Phillips: Right. So I mean obviously is a huge skill for us and Um it’s it’s not just getting the breathing tube in the ET tube in right? But also managing it and all of the physiologic changes that come with that after we intubate somebody. So it is a big part of what we do in terms of managing that airway after intubation. And, you know, a lot of the alarms are tricky and a lot of the alarms, as we’ll discuss, are not really that transparent about why they’re alarming.
Jason Hine: Yep. And I think sometimes we, we kind of, like you said, we high five ourselves, we move on. We leave the RT to do these things, which is their fantastic resource. But the over-reliance on it may lead to some skill set decay or waning knowledge base as well, where we just kind of passed the buck off, you know,
Andrew Phillips: Yeah, and you know, that’s that’s not the best way to go. We have both physiologic knowledge and we’re the physician in charge of that patient. And so we should very much be front and center and addressing any of those issues because there is something wrong causing any of those alarms. It’s something that needs to be addressed.
Jason Hine: Yeah, perfect. So, that’s my hope. Today’s to kind of address the most common alarms. My hope is to kind of do some case scenarios with you. I will, you know, for the listeners I’m gonna feign a little lack of knowledge. I know some of this certainly not to the degree of Dr. Phillips, but I will, I will play dumb for those involved and I’m gonna have you walk us through the situation. How’s that sound?
Andrew Phillips: That sounds great fire away.
Jason Hine: Perfect. All right. So you’re on shift and you intubate a patient for an acute polypharmacy ingestion. As a suicide attempt to overdose. They have a suppressed GCS. You high five yourself in the mirror of the bathroom say Man I’m a good doc I handle that airway great. You move on to the next patient. Nurse calls you 10 minutes later for vent alarms. You go in the room and you see a high respiratory rate alarm. Andrew what is what’s going on here? You know, I I set the respiratory rate at 18. Why is the machine saying that they’re now breathing 30?
Andrew Phillips: Right. So the most important question, the first address here is how long before shift change. Just kidding.
Jason Hine: And good point yeah passed the buck. Pass the buck again.
Andrew Phillips: Just kidding. So you know it’s really a misnomer and an unfortunate one as well to say that you’re setting a respiratory rate. Of course, that’s what it says on the ventilator. It’s not the respiratory rate that you’re setting realistically it’s the minimum respiratory rate because patients in any of these modes, are able to breathe above and beyond whatever that set rate is. Now I’m talking about for any kind of setting in which there is a set respiratory rate, right? I’m not talking about pressure support, I’m talking about like, AC VC and things like that. So they can breathe above and beyond, what’s really going on. If there’s a high respiratory rate is, they have an acute Propofol deficiency. I say Propofol specifically, you know, not dexmedetomidine for example, is because one of the good things about dexmedetomidine generally speaking is, it does not suppress your respiratory drive. But in this case, if they’re breathing well above the ventilator or their breath stacking or they have some sort of pathology that requires them to slow down. You have to get them to slow down their breathing. COPD would be another good example. Then you’ve got to get them to stop breathing. And the way to do that is Propofol, or one of the opioids, right? So give them some fentanyl. Give them some more morphine or dilaudid. You’ve got to give something to stop that respiratory drive.
Jason Hine: Ok. That makes sense. Yeah. So we’re gonna try to slow them down. Propofol seems to be your preferred agent. Now let’s say Devil advocate here. So let’s say that this patient ends up having positive salicylates on their laboratory work or change the patient, it’s a severe DKA. How do you manage the respiratory rate in that patient with a metabolic acidosis or another reason for that tachypnea?
Andrew Phillips: Absolutely. And this is a great example of why we should be heavily involved in addressing any of these vent alarms, because it’s up to us to understand the underlying pathophysiology of why that patient became intubated. If they’re in DKA or they have a salicylate toxicity. That is a metabolic cause of the respiratory failure, right? Their lungs generally speaking are, are okay. We’re not trying to make up for the lungs. We’re making up for the respiratory drive that was required to compensate for their metabolic problem and when it’s a metabolic problem, basically causing them to wear out, right? You have to match what they did previously. And the way to pay attention to that is with their minute ventilation. So especially what I’m talking is, you know, some of our fellows up in the ICU, trying to get them to understand how they’re making these fine tuning adjustments. When you’re seeing your CO2 or you’re trying to adjust, and compensate for DKA or something, that’s really severe like this. Don’t be looking at, just the respiratory rate, don’t be looking at, just the tidal volume, you have to look at the minute ventilation because that is what’s going to drive down the CO2. But then compensates for their lack of bicarb and all the academic processes that are going on. So the metabolic cause you have to keep up. With a respiratory. Cause you generally want to slow down and give their lungs a rest. They’re not going to have to breathe as fast for a respiratory. Cause once you give them enough oxygen, they were being fast in order to oxygenate. It’s not an option problem when they have DKA, it’s a ventilation problem and they’re getting tired. So pay attention to what the cause of respiratory failure is, and that is 100% your job, not RTs.
Jason Hine: That makes sense. And so with that acute propofol deficiency. I love that term if we’re talking about pneumonia COPD, another reason. Once we get that, you know, hypoxia addressed we can we can drive their respiratory rate down by suppressing it, but you’d probably put yourself in a bad place if you were suppressing the drive in someone who has a metabolic acidosis, so keep up with it in that circumstance.
Andrew Phillips: Yeah, you’re gonna see that pH drop really fast if you’re not careful. And remember those are the patients who they already have a low pH a 6.9 sometimes 6.8, you know, there’s a debate about giving bicarb when you intubate and that’s a whole other conversation but those the patients who right if they’re already 6.9 and you go make them go apnic for a moment while you’re intubating, baby, you got to keep off because you’re gonna find that 6.9 to 6.7 really fast
Jason Hine: Yes, the whole resuscitate before you intubate. That is an important process for sure. All right so next patient you move on to your very next patient and you intubate a polytrauma patient who has significant face facial injuries. Eight minutes later now you get a new vent alarm it states, air leak. Andrew. What’s going on here?
Andrew Phillips: Yeah. So we’re discussing this pre-production here, just going over cases, we’ve had and, and how frustrating it is to get that tube in and then to realize that tube’s not working all that. Well, so the air leak is when you have a closed circuit. So, this is a secure airway, an ET tube where it is measuring of course, the amount of air that comes back and it gives you a sense of leak because it knows how much air went in with the volume in was and what the volume out was. And if it’s not detecting the air coming back then it’s going to alarm that there’s an air leak. Air is going somewhere other than back into the ventilator and really that’s going around the ET tube somewhere, and it means you’re cuff is not working. Maybe this person has a history of tracheomalecia. You need to move the location of the balloon or in this case was significant facial injuries and unfortunately, probably got nicked by a tooth, or an exposed bone on the way down. And so you’re cough, just no longer will hold air.
Jason Hine: Okay. And you’re gonna see that alarm as an air leak specific alarm or maybe a low tidal volume alarm or loss of peep. Is that how that might manifest?
Andrew Phillips: Yeah, exactly. So your title volume going in is going to be the same. You’re gonna end up losing peep because, you know, the vent has to have that balloon up in order to hold that air in the lungs. And, you know, if you lose that balloon, you lose the ability to keep that air in the lungs. And so, you’re going to to see that the peep is is coming down. It’s gonna be set at a certain amount but you’re not actually going to achieve that deep and you might see that alarm as well.
Jason Hine: So air leak alarm or losing peep alarm both, need to take a look at your balloon. Take a look at your tube location.
Andrew Phillips: Absolutely.
Jason Hine: All right, okay. Okay. Next. Next patient. We got a busy day here in our emergency department. Your next patient is a Yeah…
Andrew Phillips: Never heard of that.
Jason Hine: Your next patient is a severe asthma attack and they’re losing mental status. You intubate them. Six minutes later. I don’t know if you notice, we went from 10 minutes later to eight minutes later, it’s getting faster and faster. These event alarms are coming at us hot. Six minutes later, you get a vent an alarm high peak pressure. Andrew what is happening and what do you do?
Andrew Phillips: Oh, the asthmatic, boy. Try not to intubate these people, right? A lot a lot…
Jason Hine: Yes. Yeah.
Andrew Phillips: A lot goes wrong with the asthmatic and the COPDer when they get intubated. And so let’s let’s talk about that and it for me, it has to we have to drive a little bit into the physiology side of things. So got to scrape back in the med school days and you know, there’s an important difference between the peak pressure and that’s what’s going to alarm the peak pressure, which is the highest pressure. It’s a dynamic pressure, anytime during the course of breathing, this alarm will go off. If the pressure that’s set is too high and this could be any cause it could be my fat foot stepping on the, you know, extension of the, the ET tubing, right? Going into the ventilator that can cause a high peak. It can be any of that stuff. The other pressure, you need to worry about, is the plateau pressure. And for those who aren’t as familiar with this, the plateau pressure is a static pressure and it’s an inspiratory pause. So, during a breath, you actually have the vent hold the breath. It will measure the pressure at that point, which takes away all of the flow issues, so in an asthmatic, right? The bronchi are very inflamed, they’re very small. The flow is causing a high pressure because those tubes are more narrow. So, gross way of thinking about this is that the peak pressure Is usually something just along the tubes, right?: Whereas the plateau pressure is what is being felt by the alveoli. So the peak pressure will go up and then you have to ask yourself, Is this a high peak pressure with a high plateau pressure? Meaning, something’s wrong with the lung parenchyma or something with the alveoli itself versus a high peak pressure and a normal plateau pressure which is what happens, consistently in asthma and to a similar degree in COPD. Although usually a little less on the high part there but it’s very common, for example, in an asthmatic patient to have high peak pressures and the 80s 90s and someone who’s in status asthmaticus, right? Really really bad asthma, requiring intubation but their plateau pressure because they’re alveoli are fine is going to be normal. Now, one thing I want to add to that and we should circle back around this. At this point with this asthmatic and this is a whole other conversation, right? But with this asthmatic, that high peak pressure alarm Is stopping your breath. And I think it’s important enough to say that again that when you have a high peak pressure alarm, this is often ignored by people, not just the physicians but the nurses who are bedside, even some RTs. The breath is actually being stopped the tidal volume, you set, as the minimum tidal volume is not being delivered, whether it’s a high peak pressure larva, it’s a safety mechanism because event thinks it’s gonna blow up the alveoli. So you’re gonna wind up with this patient, I guarantee not only having the high peak pressure alarm, but also the low minute ventilation alarm because they’re not getting the breath. And you’re about to go from someone, who’s just hypoxic to also hypercapnic and you’re gonna get into a hole that’s really difficult to get out of. I know, that’s a lot of explanation I just gave for one simple question, but they all tie together. So high peak pressure, the first question should be asking yourself, is “Is the plateau pressure high or is the plateau pressure normal?” We should definitely recap that because it is a mouthful.
Jason Hine: Yeah. Yeah, that’s super important to go back over and I mean, we could have a whole other conversation on intubating the asthmatic. You know, I’ve been taught and I tell my residents, intubating asthma is varying degrees of failure, right? We’re trying to do not that as best as possible,…
Andrew Phillips: Yeah.
Jason Hine: And that is kitchen sink, right? Your magnesium, your epinephrine, everything you can give that person the stave off intubation, you need to do, but sometimes, unfortunately, they need to be intubated. And so going over when you get these high peak pressure alarms, we’re going to want to first ask ourselves, what is the plateau pressure? And that’s going to help differentiate root cause just a little bit. In patients, with the high peak normal plateau, which is common in asthma because of the bronchospasm and normal alveoli, that that’s a common scenario that we’ll see. Other reasons, just kind of going over potential causes you mentioned. You know, if you’re stepping on the extension tubing at the end of tracheal tube is kinked at the mouth or the bite block. Maybe, I don’t know a mucus plug. Would that be another reason? Or like if you got a bunch of gunk or blood stuck into the endotracheal tube, would that be another reason for a high peak normal plateau?
Andrew Phillips: Certainly very much so and not just the kink I would add a very common one. Yes, kinking at the bite block but before you put the buy block on then biting down on the tube they’re starting to wake up can cause it really one way to think about the high peak pressure and normal plateau is tubing some sort of tubing. It’s bronchospasm at the the lung level. It is biting at the mouth level, it’s someone stepping on the tube or the wheels rolling and I say that in someone’s probably thinking Gee I never feel it. Step on the tube. I have seen those wheels roll onto the extra long tubing, right? Like you have to run your circuit. I’m sure we’ve all been amazed at the stuff that can go wrong that you wouldn’t think of until you see it and this stuff absolutely happens.
Jason Hine: That makes sense. Yeah. You like to think we’re above that but we are certainly not. And then so the other type
Andrew Phillips: Murphy’s Law.
Jason Hine: Exactly… What can it will.
Andrew Phillips: Yep.
Jason Hine: So high peak high plateau. So then this is less of, you know, I think almost for the high peak normal plateau, someone taking a kelly’s and and clamping something. It could be intrinsic to lungs. It could be in the ET tube. It could be in the tubing. We went over that. In the high plateau circumstance, the lungs aren’t really moving or opening properly, in some capacity that could be you took out one of the lungs. Maybe you’re only working with the right because you main stemed them and unfortunately, this I guess could happen in asthma. If they breath stack and they pop a pneumothorax and start getting tension physiology, these are reasons why it might be a high plateau high peak. Is that correct?
Andrew Phillips: Yeah, I would agree with that and this is why I love your asthma example because your point of breast stacking. We’re now talking about high peak pressure and high plateau. We’ve gone into the decreased compliance. So, so for a second for the physiology nerds the high peak pressure with the normal plateaus you’re increased resistance. The high peak with a high plateau is your decrease compliance and asthma, just fit both of those. And so you have to be careful in the beginning. This patient, as you first describe, six minutes after intubation falls into the increased resistance problem. It’s just the asthma, but you’ve got to keep watching that plateau pressure because if it starts to rise, now you’re thinking breath stacking right? Now they’re auto peeping, or they pop the pnuemo. So asthma can jump between these and Honestly, if you’re not familiar working with these patients and and tubing them very often is a good time to phone a friend.
Jason Hine: Yes, yes, exactly. Calling your resources work with your senior RT as well as your ICU docs. And so if you do start to get in that category, you know, High Peak normal plateau, we’re doing everything we can to get that albuterol in, if we’re on an EPI drip, that’s probably a good idea. We’re doing everything we can for the bronchospasm. if we start moving into the high peak high plateau, that’s the time where you might consider disconnecting, the patient, from the ventilator momentarily, putting some pressure on the chest to allow for a full exhalation, and maybe taking your ultrasound out and making sure you’re still have lung sliding.
Andrew Phillips: That is an amazing feeling when you do that and it works. I mean routinely what I’ve had to actually set my phone alarm on one patient, a particular, I’m thinking of every hour I was having to go in there. This is already admitted from the ED. So you wouldn’t have to keep this up, but he was in the unit. And I had to set my alarm for every hour to remind myself to go into his room. Disconnect the ventilator press on his chest. And his MAP, would immediately jump. It’s a MAP not just systolic. MAP, would jump, seven, right points every hour and at first, you know, staff is little nerved by this by the seventh grade time. It’s like, Hey Dr. Phillips, welcome back. How you been? and, Yes,…
Jason Hine: Kind of push on that, that gentleman’s chest? Yeah.
Andrew Phillips: Yes, and I, I look back and smile at this, because everything went fine with him. He did great, but it was, you know, that’s how bad it can get.
Jason Hine: Yeah. Certainly. So coming back around to that, a little bit of a nuance point about the, the peak pressure, the alarm and the truncation. So, you know, we do think about sort of tidal volume respiratory rate as our means of controlling CO2, think about the oxygen delivery and the peep for hypoxia but you mentioned something that’s important to circle back on when you’re getting these high peak pressure alarms you are getting truncated breaths so you’re not delivering your full title volume and…
Andrew Phillips: Correct.
Jason Hine: you need to be cognitive that of that and keep an eye on what your CO2 is doing trying to allow for full delivery of that title volume correct?
Andrew Phillips: Yes, very important detail and that’s all ventilators I’ve ever heard of.
Jason Hine: Okay, excellent. All right, so let’s wrap this up. I’m gonna give you the alarm that happens and sort of you tell me what’s going on physically and how we as physicians can fix it? How’s that sound?
Andrew Phillips: I don’t have to form an answer in the form of a question, right?
Jason Hine: You do not.
Andrew Phillips: Bonus points.
Jason Hine: So First one, we mentioned high, respiratory rate.
Andrew Phillips: Propofol deficiency.
Jason Hine: All right, that’s easy. That one’s quick, remembering again that we set the minimum respiratory rate, not the maximum, the patient can drive the maximum, and we’re gonna suppress respiratory drive When we don’t think that there’s a metabolic problem going on, we’ll let them continue to respire at the rate that their bodies needing to, if we’re talking, you know DKA, salicylate toxicity were the examples.
Andrew Phillips: Certainly and you mentioned since we’re gonna add a bit to it, you mentioned propofol seem to be kind of my go-to. Yes. In the sense that often when they have a high respiratory rate they’re very agitated, so their blood pressure tends to rise. So you can hit converts with one stone by using propofol both sedating them dropping the respiratory rate, and reducing that blood pressure. But if they happen to be breathing quickly, and you don’t have a lot of blood pressure to work with you, of course, need to go with something else. Probably fentanyl.
Jason Hine: Ok, perfect. Good nuance point there. Next alarm we talked about was air leak.
Andrew Phillips: Which is a cuff deficiency either. It’s popped a little bit or it’s popped all the way something is wrong or or the confidence is not sitting in the right place, but there is something wrong with the cuff and the way to check that is to just squeeze the pilot. It should hold.
Jason Hine: Okay, and if it’s not, we have to consider doing an exchange.
Andrew Phillips: Yeah, and you can try to get by usually when this happens it’s immediately after maybe there’s something else going on, I usually will try to put another five or 10 CCs of air into it. And then within a few minutes they’re obviously seconds. If it’s really popped it just goes away but if you’re tight on time you can usually buy yourself a little bit and then also gives you an opportunity to if you put a little bit of extra air into it, It’ll tell you quickly whether it’s just some sort of tracheomalacia or some anatomical issue. Just be sure if you add more air into that, you have to get a manometer that RT should have maybe they whether or not they have it in ED depends on your ed. But for sure, in the ICU they should have a manometer and theometer even has all the red and green, you don’t have to worry about the numbers. It’ll tell you just look at the manometer, I don’t want to bore you with those details.
Jason Hine: Okay. Yeah, I mean a brand that’s commonly thrown out there’s a posey cufflator. What are you trying to watch for in terms of your your high pressure on your your balloon?
Andrew Phillips: Yeah, so if you are trying to put in more air in there, you don’t want to over inflate because eventually it can cause some necrosis of the mucosa there. For a little while and eating, it’s not a big deal, but you want to be careful.
Jason Hine: Sure. Any specific number that you throw out for people or is it a case specific?
Andrew Phillips: Around 30. Yeah, a little less than that.
Jason Hine: 30. Okay. All right, so we did did high. We did a high respiratory rate, we did air leak. So now we have high peak pressure and a normal plateau pressure.
Andrew Phillips: Right. So, these are going to be your increased resistance problems. And I’m labeling, this an alarm deficiency because it’s not telling you what the real problem is. Except of course, you have to worry about the decreased title volume that’s going in. So the increase resistance category includes things like the circuit blockage, a kink including something in the ET tube, the patient fighting down on it. A mucus, plug, a blood clot in the bronchus, or the bronchial or bronchospasm, like, in the asthmatic example, we had. That’s a high peak pressure, normal plateau, the alarms, just going off doing its thing for something it’s not necessarily in and of itself a problem. But you have to address so that you get your full title volume.
Jason Hine: Excellent. And then, the last one we talked about was high peak pressure with a high plateau pressure.
Andrew Phillips: And this is a problem, right? This is an actual pathophysiologic problem of the lungs, you’re talking tension pneumothorax breath stacking could be really bad ARDS. Yes, could be as simple as a main stem intubation. I wish the many times that I’ve seen these. That was the problem because it’s a very simple fix. But if you’re looking at bad ARDS, you’re looking at breast stacking, you’re you’re in for a heap of hurt. So, really pay attention to those high peak pressure high plateau, you prepare yourself to spend a while by the bedside to work that through.
Jason Hine: Ok fantastic and so let’s hit these really quick at high level for us as a wrap-up for people to keep this in mind. Our four alarms, we talked about high respiratory rate, we’re going to call that an acute propofol deficiency so long as it’s not a metabolic acidosis. Air leak as a cuff deficiency. High Peak Pressure, Normal plateau is an alarm deficiency or think about a Kelly being clamped on something in the circuit. High Peak Pressure, High plateau pressure is a compliance problem and a pathophysiology that you have to really dive into. How’s that sound?
Andrew Phillips: That’s pretty good. One out of four is a real big problem.
Jason Hine: Yeah, yes one out of four is a big problem, but where the be aware, and fear the asthmatic, be ready for your breast sacking, think about your pneumothorax and aggressively treat those patients. They should certainly be using the full kitchen sink, including epinephrine. Andrew, thank you so much for joining us today sort of break down these common ventil arms. I feel more prepared for managing the vents. I hope our listeners gained a lot from it because I certainly did.
Andrew Phillips: I was my pleasure. Thank you for the invitation.
High Respiratory Rate Alarm
Dr. Phillips points out that this is really a misnomer. The respiratory rate we set on the ventilator is the minimum respiratory rate. This is the lowest rate the patient will be “allowed” to breathe before the vent steps in and delivers a breath. The patient may very well breathe above that rate.
Dr. Phillips describes this circumstance as simply an Acute Propofol Deficiency.
In this he means that you can further suppress the patient’s respiratory drive through medication, typically Propofol or an opioid. This works for most patients, particularly those with hypoxia driving their tachypnea (COPD, PNA, etc.).
Caveat: If the patient’s pathophysiology demands a high respiratory rate (ex DKA or salicylate ingestion causing a metabolic acidosis) we as the clinician must be aware of this and address the minute ventilation.
Air Leak Alarm
When you have a closed circuit for ventilation, the vent measures the amount of air that goes in and comes back out. With the Air Leak Alarm, air goes in, but is not coming back. This usually means the air is escaping somewhere.
You can think of this simply as a Cuff Deficiency.
In the case we discussed of the polytrauma patient, this means the balloon likely got nicked on a fractured tooth or exposed bone. This can also happen in cases of tracheomalacia or abnormal anatomy. The solution is to replace the tube if the balloon will not hold air or reposition the tube in the case of tracheomalacia.
High Peak Pressure Alarm
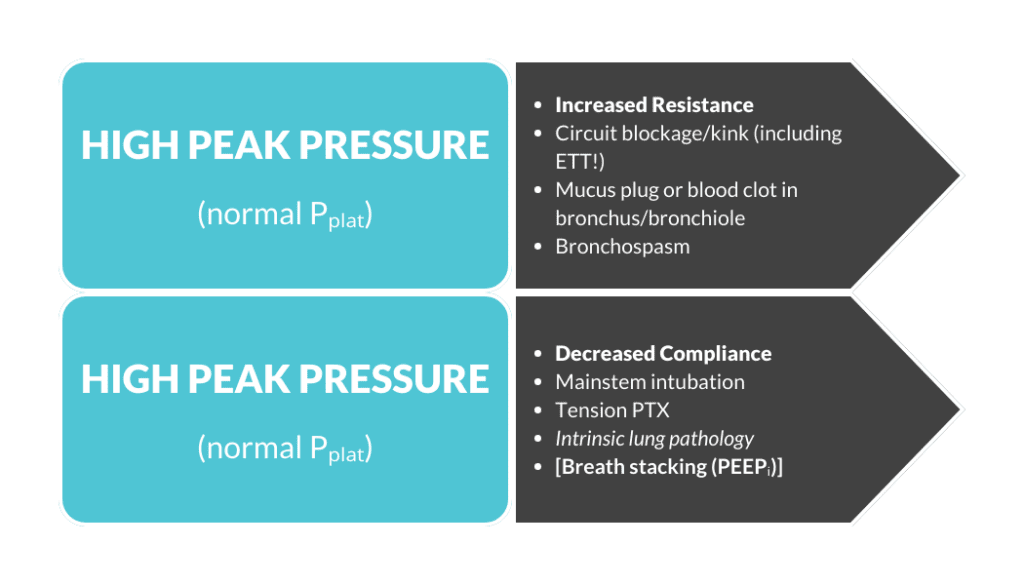
This measures the amount of pressure that is occurring while the tidal volume is being delivered. This is a measurement of the pressure along the system. Where in the system this is occurring is important to figure out, as different types have different solutions. When the High Peak Pressure Alarm sounds, the next question you should be asking yourself, per Dr. Phillips, is “what is the plateau pressure?”
High Peak, Normal Plateau Pressure
This can be thought of as “high resistance,” which can happen when flow is limited in an area of the tubing. If you step on the ventilator tubing, for example, this alarm will sound. It will also occur if the endotracheal tube is kinked at the mouth. Mucous plugs and bronchospasm of asthma are also potential causes.
High Peak, High Plateau Pressure
This can be thought of as “decreased compliance”. The plateau pressure represents the amount of pressure felt in the system during an inspiratory pause. This is the amount of pressure that is felt by the alveoli. It can happen, for example, if you right main stem the patient or the patient blows a pneumothorax. Or again in asthma, the patient is breath stacking.
Check out the graphic below which helps clarify this “High Peak, High Plateau” pressure differentiation.
Peak vs. Plateau
Summary
These three common alarm types can be summarized simply as:
1. High Respiratory Rate – Propofol Deficiency
Caveat: Watch for metabolic acidosis or other reasons the patient needs a high respiratory rate
2. Air Leak = Cuff Deficiency
3. High Peak, Normal Plateau = Increased Resistance
4. High Peak, High Plateau = Decreased Compliance
Practicing procedures can be tough. Let SimKit do all the heavy lifting in your skill maintenance. Procedural training can and should be easy, done in your home or department, and work within your schedule. We want you to be confident and competent clinicians, and we have the tools to help.




