Hello everyone and welcome to the Simkit podcast. I am here as your host, Dr. Jason Hine. Today we are going to be talking about central lines and we’re going to spend a fair bit of our time talking about the subclavian line and why I believe it is the line of champions. So with regard to central access, there’s generally a when and a where for this, right?
And I would argue that we in emergency medicine know the when quite well, whether they are incredibly sick with hypotension and need vasoactive agents like pressers. That’s probably the most common reason. Hemodialysis, there’s a laundry list of indications, but we know the when. Well, the where is where we want to focus our attention today. And generally speaking, there are three points of axis that we consider for obtaining a central venous catheterization the ephemeral, the subclavion and the internal jugular.
And I would argue that we all have our default, our go to. We have that one location that is preferred and we only stray away from that when the patient circumstance does not allow us to use that point of access. But what is that default for most of us? I would argue that across the country the most common point of access for central catheterization is ultrasound guided internal jugular. That is probably the most commonly used location for central catheterization in emergency medicine.
But is it what we should be doing? Well, what do the guidelines say? What recommendations from national societies do we have? What does the CDC, the center for Disease Control and Prevention say when it comes to location for central venous access? Well, they make the following recommendations.
They say, quote use a subclavian site rather than a jugular or femoral site in adult patients to minimize infection risk for non tunneled CVC placement. A category one B recommendation. And this is from their Guidelines for the Prevention of Intravascular Catheter Related Infections from 2011 with an update in 2017 subclavion that is not, as we discussed, likely what most of us are doing now. Why is that? Now, I like to think, and this is a generalization, but I think many of us think of the IJ as easy, the subclavian as complicated and the femoral as dirty.
Now, as an aside, we’re probably seeing some data that the femoral is not as dirty as we thought, but certainly with our increasingly obese population, with the overhanging panus, that can often be a difficult site to keep clean. But this speaks to a more global point, that when we are picking our location for central venous catheterization, we have to weigh the risks versus the benefits. Now, what are the risks? Now, for risks we need to consider things like arterial puncture, infection, thrombosis, hematoma, damage to dangerous things surrounding the vein and of course, failure of the point of access. On the other side of the coin, the benefits to consider are cleanliness, low thrombosis risk, compressibility of the site being away from these dangerous things and of course, success.
Now, outside of this CDC recommendation of the subclavian line mostly for infection prevention, what data do we have about the specific risk and benefit profiles for these three sites? Interestingly. I think the highest quality data we have to date comes from the three sites study group and their article in the New England Journal of Medicine titled Intravascular complications of central venous catheterization by insertion Site published in September 2015. Now, this was an ICU based study. So in full disclosure and understanding of our literature, we need to recognize that this is not our ed population, but it is covering a topic matter and a procedure that is relevant to our specialty.
In this study, patients were randomized to one of three sites the IJ, the Femoral and the subclavian. When able to, they were randomized in a one to one to one fashion. When one site was excluded for one reason or another, they were randomized in a one to one fashion. During the one to one to one randomization. There are about 850 catheters for each location.
So this is a large, well done study. It is important to note here that the landmark technique was used a lot for the subclavian. It was used 86% of the time for Ephemeral 74% and even the IJ one third of the time. A landmark technique was used in this 2015 study. Rather interesting.
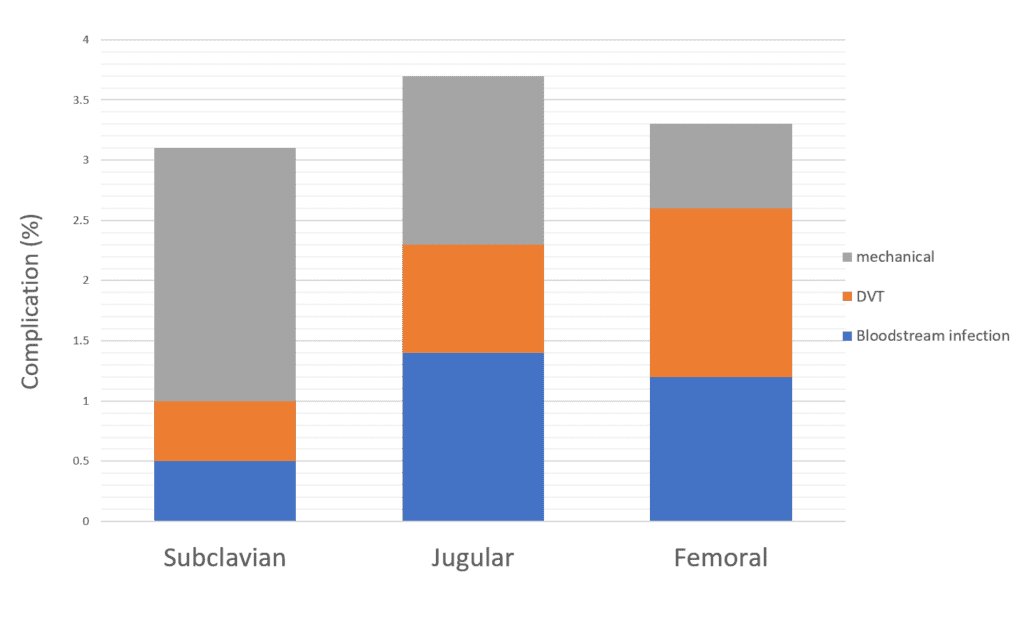
So what were the study results? What did they find? They broke down complications into mechanical thrombosis and blood stream infection. When complications were taken in aggregate, they found that the subclavian line had the lowest collective rate of complications. That is, despite it having by far the largest mechanical complication rate, it’s not hard to deduce then that it had much lower rates of thrombosis and infection.
Now what if I told you there was a fantastic way to decrease this mechanical complication rate with a skill set you already possess to make the subclavian line by far the most advantageous with relation to its complications? Enter ultrasound guidance. And there is data supporting the use of ultrasound for subclavian central venous catheterization. Now, it is plagued by many of the same difficulties that much of the ultrasound literature out there has, including small sample size, having a very experienced or fellowship trained operator, et cetera.
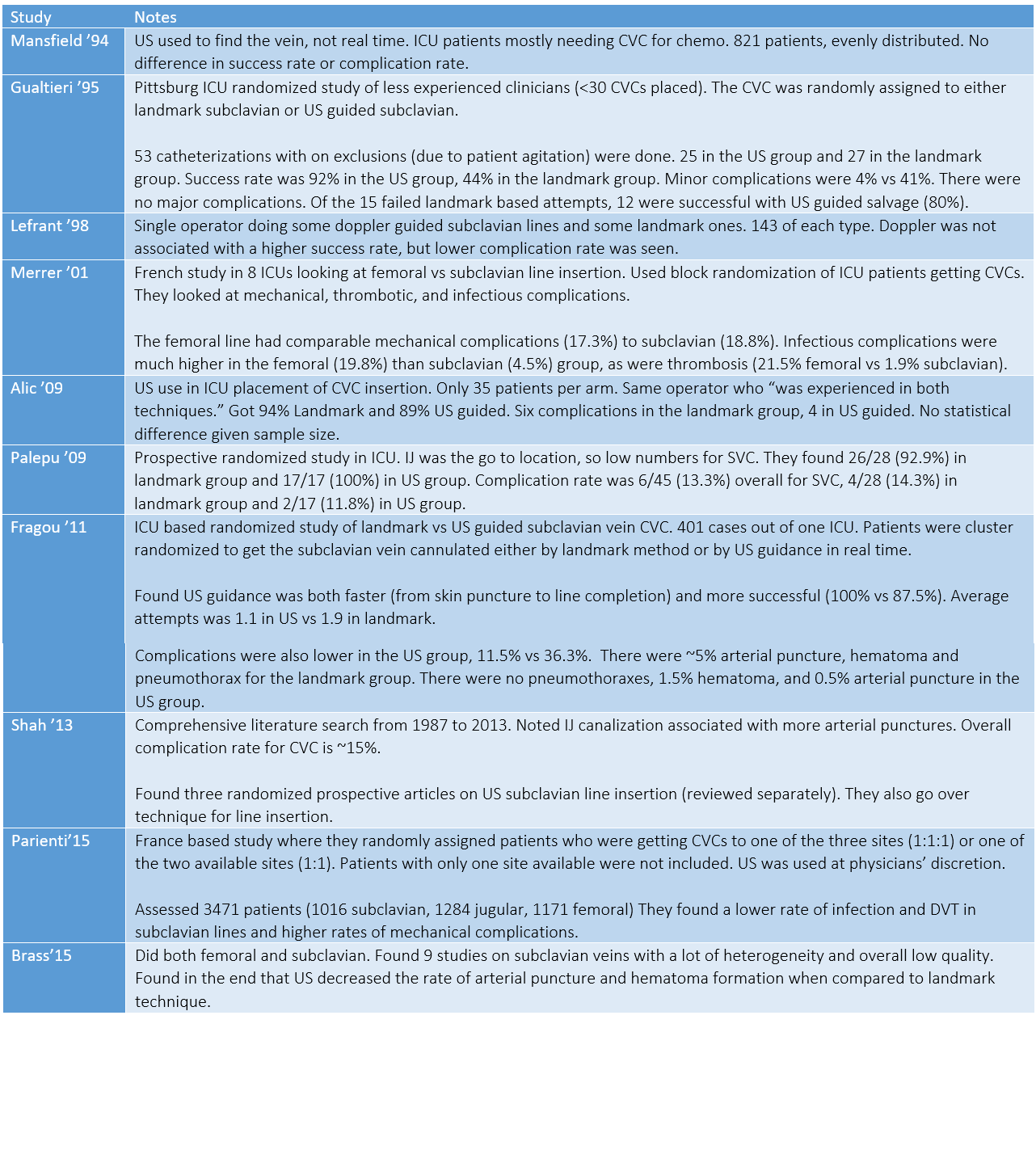
That said, the study I would most want to highlight in this conversation is The Cochrane review in 2015 by Brass et al titled “ultrasound guidance versus anatomic landmarks for subclavian or femoral vein catheterization.” Now, in this Cochrane review, there were 13 total studies, nine of which reviewed subclavian catheterization. Of these nine studies, four used doppler, five used two-dimensional ultrasound. One of these five used ultrasound only for identification. The other four used real time ultrasonography like we do currently. The publications ranged in year from 1994 to 2011. What was the end point of this Cochrane review? Their conclusion was that ultrasound offers small gains in safety and quality when compared to the landmark technique. Now, you might be thinking to yourself that is not a very strong endorsement from the Cochrane Library. Well, first of all, I would say that that’s fantastic small gains in safety and quality is what we’re looking for every day in the care of our patients. And secondly, if you allow for a little personal interpretation, possibly with my own personal biases, I think that this final recommendation slightly skews away from the utility or benefit of ultrasound. As I mentioned, these studies go back to 1994. We are getting way less comfortable with landmark or anatomy-based procedures and way more facile with the use of ultrasound in our procedures.
I believe in the modern era, with the migration of our skill sets toward ultrasound based and away from landmark or anatomy based procedures, that small gain is likely much larger.
So then the next question becomes how are we doing this? In actuality, how are we gaining access to the subclavian vein via ultrasound? Now, as a refresher, when we are gaining this access via landmark technique, we are finding the junction between the medial and mid one third of the clavicle and sneaking under the clavicle itself to gain access to the subclavian vein. Now, the dirty little secret to the ultrasound guided subclavian vein is that we are often identifying, tracing, and even doing our vena puncture in the axillary vein, which is, again, that name change in the vessel when the subclavian passes over the first rib to become the axillary. Starting out laterally, identifying the axillary vein and tracing it inward and upward toward the clavicle. Sometimes, depending on the localization viewpoint and safety of point of access, that is also where we are doing our venipuncture. So how do we do this in actuality? What are the steps or micro skills involved in the ultrasound guided subclavian? Well, first recognize that you can do this in the cross sectional or longitudinal approach depending on your comfort level. I have a greater skill set with cross sectional, but there is definitely some information or data to suggest a longitudinal approach allows better localization of your needle tip and avoids some Transection of the vessel or injury to posterior structures.
Regardless of your cross sectional or longitudinal approach, you are taking the probe, putting it out very laterally on the chest at the intersection between the pectoralis muscle and the deltoid. The probe down in cross section here almost in the axilla and sweeping from lateral to medial. For our anatomy identification, we are going to recognize the pectoralis muscle and the axillary artery and axillary vein as we move lateral to medial. We are also going to move cephalad toward the head and toward the clavicle. Eventually this vascular structure will dive under the clavicle itself. As we are doing this sweep, we are looking for the largest venous target that is furthest away from the pleura as possible. This is where we are going to be doing our venipuncture.
Now, this is very visual and in our show notes and on our websites we have many freeze frames, anatomical depictions as well as videos of this anatomy on ultrasound. Highly recommended that you review this. So to state those steps, again, we are taking our probe and putting it out between the intersection between the pectoral and the deltoid muscle. Really almost out by the axilla. We are doing a cross-sectional sweep looking for the anatomy that includes the pectoralis muscle and the axillary artery and vein beneath it. As we move from lateral to medial, we are tracing these vascular structures and watching them as they dive under the clavicle. We are looking for the largest venous target that is furthest away from the pleura as possible. This is where we are going to be doing our vena puncture, either in the longitudinal or cross-sectional plane. Now, if you are having a difficult time finding a structure that can be safely cannulated, there are a couple tricks you can do.
You can place the patient in Trendelenburg, which may dilate the vessels further, and you can have the patient’s shoulder brought into a shrug position, which moves the clavicle up out of the way and allowing the axillary vein and subclavian vein to be more easily viewed. There’s a great post on PulmCrit about these shrug technique, which again is referenced in the show notes.
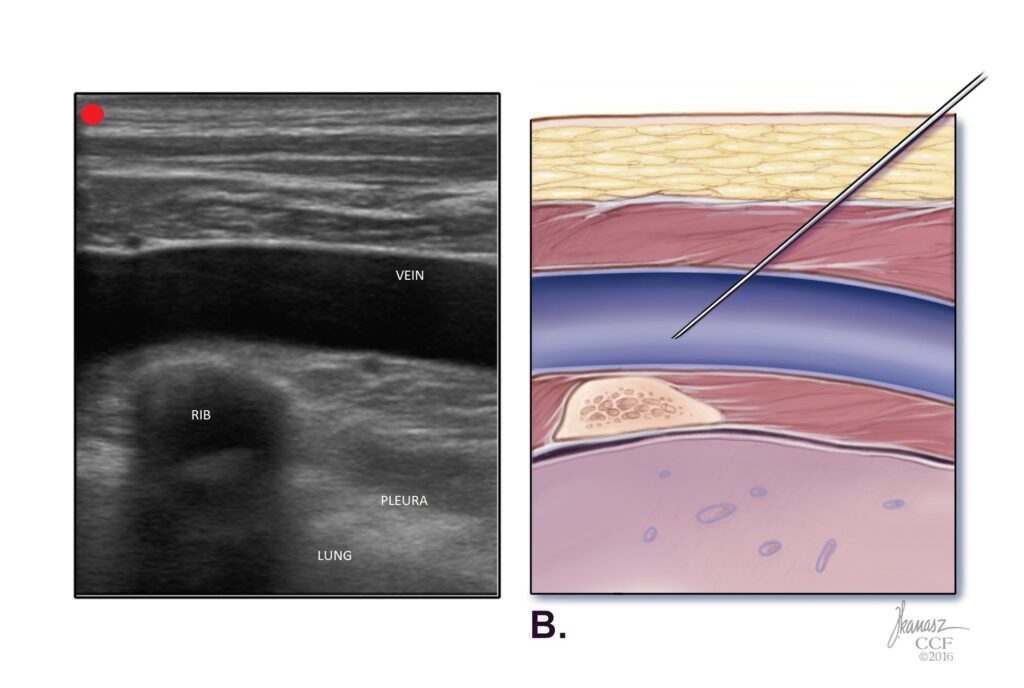
Now for completeness sake, we also want to mention the plural avoidance with rib trajectory or PART technique, which is highlighted by Dr. Senussi’s publication in the Journal of Intensive Care Medicine in 2017. With this technique, you’re essentially identifying the second or third rib and really using it as a backstop to prevent any potential for plural penetration. Certainly a pro move for those who are facile with ultrasound.
What about landmark based subclavians? There are certain times in crashing patients when a landmark based central venous catheterization needs to be placed. In trauma we are often thinking about the subclavian or the femoral because of C collar placement, precluding use of the IJ. As a refresher for the landmark-based technique infraclavicularly, we are typically finding the junction between the mid and medial one third of the clavicle and sneaking our needle under the clavicle to gain access to the subclavian vein. Another approach that must be mentioned is the “pocket shot” or the supraclavicular approach. In this approach, the patient’s head is turned away from the side of access and the practitioner is palpating the lateral boarder of the sternocleidomastoid muscle and its intersection with the clavicle. At this point of intersection, there’s a soft tissue indent, or the pocket. Once this pocket is identified, the needle is inserted one centimeter lateral to lateral head of the sternocleidomastoid muscle, and one centimeter posterior to the clavicle, aiming for the contralateral nipple.
A meta-analysis by Chen et al. in American Journal of Emergency Medicine 2020 compared the supraclavicular and infraclavicular approach for landmark based subclavians. In this meta-analysis, including eight articles from 1982 to 2018, they found the supraclavicular approach outperformed the infraclavicular approach in general with relation to failure rates and complication rates, in particular pneumothorax.
Okay, this was a short but action-packed episode of the SIM kit podcast. Let’s do a quick summary before we warp up. We talked about the three most common sites of central venous catheter insertion, including the ij, subclavian, and femoral. I made the argument that across the country, the most common point of access is the ultrasound guided IJ, but pointed out that the subclavian site, rather than the internal jugular, is the site recommended by the CDC, at least with regard to prevention of infection. We then went on to go over some of the data for and against each of these locations, particularly focusing on the Three Sites trial that showed that collectively the subclavian has the lowest complication rate and the majority of complications for subclavian were mechanical in nature.
Then went on to talk about how we could potentially decrease this mechanical complication rate by using ultrasound guidance. We reviewed the Brass at al. Cochrane review on ultrasound guidance for subclavians, who noted a small gain in safety and quality when using ultrasound over landmark technique. I made the argument that in the modern day with our increasing ability and skillset with ultrasound, that is likely an understatement of the potential benefit. We went on to review the practical steps of doing an ultrasound guided subclavian cannulation, talking about starting in the cross-sectional view for anatomy identification along the pectoralis muscle and the deltoid way out by the axilla, where we are recognizing the axillary artery and vein and tracking those vessels as they move immediately cephalad and dive under the clavicle. Anywhere along that course where we have a large venous structure that is relatively far from the pleura, we have the opportunity for cannulation.
Again, this can be done in cross-sectional or longitudinal approach depending on the operator’s comfort with each. We mentioned placing the patient in Trendelenburg or using the shrug technique to improve our visualization, and we talked briefly about the plural avoidance with rib trajectory or PART technique where we use the second or third rib as a backstop for a cannulation. And then we concluded with a final brief discussion about how if we need to do a landmark based technique, we may want to consider the pocket shot approach. So as we come to a close, I again want to mention the amazing show notes that accompany this podcast. It has not only the primary literature, which you can review on your own, but also freeze frames, anatomy depictions, and video of how to do this ultrasound guided subclavian. Thank you so much for listening. Until next time.
Which central line is best? I would argue we all have our “go to” line, which across the country is likely the ultrasound (US) guided internal jugular or IJ. Well, considering common circumstances encountered by Emergency Medicine (EM) clinicians, what does the literature say is likely the best line??
To answer this question let’s dive into the literature… I think you’ll be surprised by what we find.
Society Recommendations
Between the IJ, subclavian, and femoral line, when everything else is equal, which is recommended by professional organizations?
The Center for Disease Control and Prevention (CDC) makes the following recommendation:
“Use a subclavian site, rather than a jugular or a femoral site, in adult patients to minimize infection risk for non-tunneled CVC placement. [Category IB]“
Where does this recommendation come from? They base it on three studies: [Merrer 2001, Goetz 1998, Robinson 1995].
This analysis brings up a more global point that for each line and site we need to weigh the risks and benefits. These potential risks and benefits are shown in the figure below:
Aside from the CDC recommendation, what other data do we have to guide our decisions on what site is best? The most valuable data on the topic comes from the 3 SITES Study by Parienti in the New England Journal of Medicine (2015). They compared the IJ to subclavian to femoral in a 1:1:1 randomization fashion. When looking at complications, they found the following:
The subclavian line had the lowest overall complication rate at just above 3%. As you can see, the majority of these were mechanical.
Enter Ultrasound Guidance
What if we could decrease the mechanical complication rate with a skillset we already have? What if the graph looked more like this?
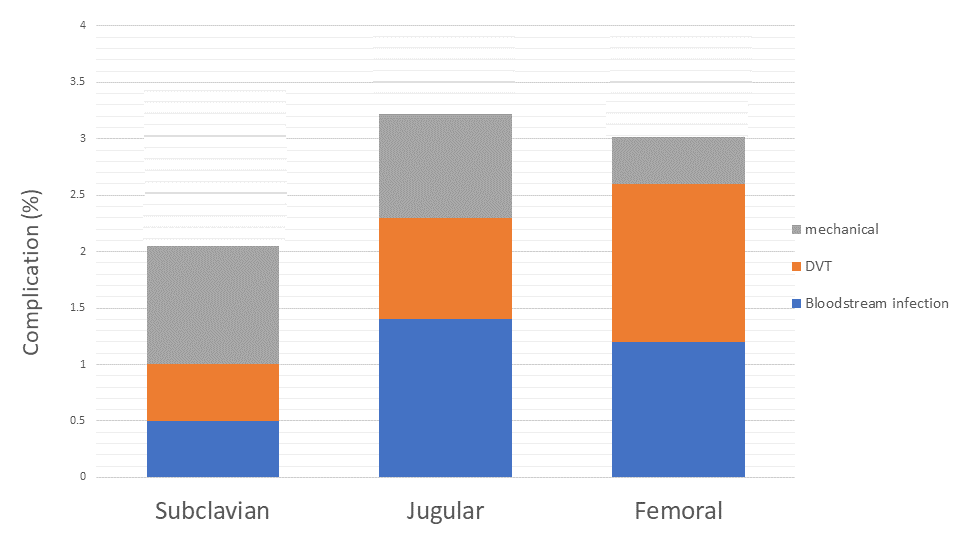
Notice how all three have a decrease in mechanical complication rate, but it is the subclavian’s much lower thrombotic and blood stream infection rates that really lead to the difference. The use of ultrasound can achieve this in the right setting and with the correct skill set. This is supported by the literature.
A Cochrane Review in 2015 reviewed 9 articles on the use of US for subclavian lines, 5 of which involved 2 dimensional US (4 using doppler only). In their review they concluded:
“US offers small gains in safety and quality when compared to landmark technique.”
While this is not a glowing review, I think it likely under estimates the true benefit in modern practice, we we are getting way more comfortable with US and much less facile with landmark or anatomy-based procedures.
Some of the relevant supporting literature for US guided subclavian line is summarized in the table below. See reference list below for all studies.
How to Perform an US Guided Subclavian Central Line
The secret to the US-guided subclavian CVC is to look much more laterally than the landmark technique. In the landmark approach, we are finding the junction of the middle and medial thirds of the clavicle, then sneak our needle in under the bone to hit the subclavian vein.
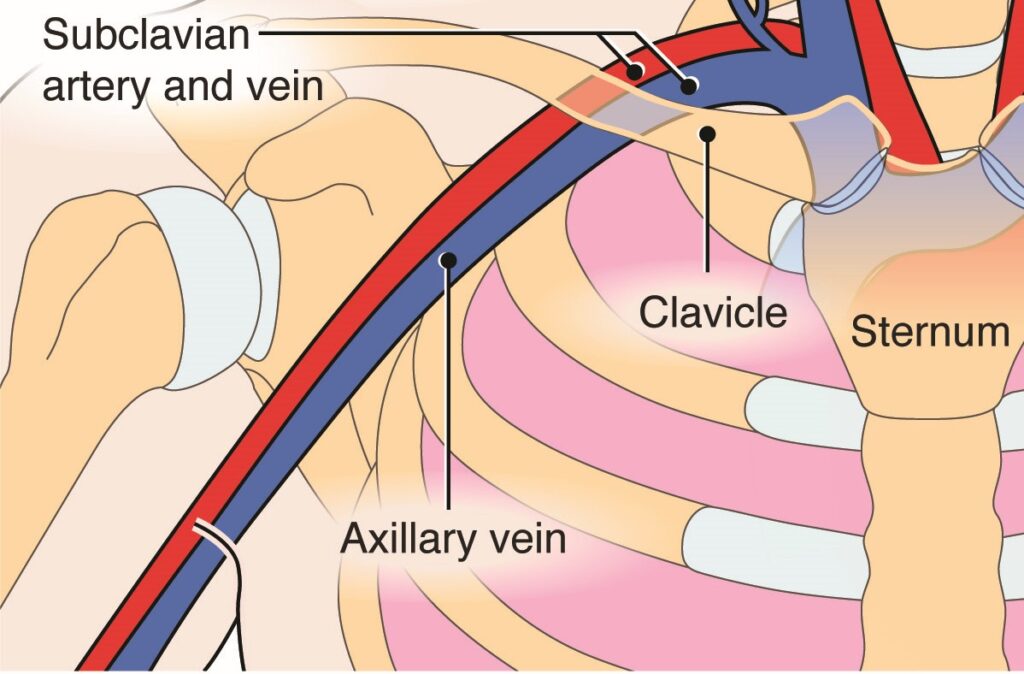
In our US-guided approach, we start laterally to identify the axillary vein and find our ideal venipuncture site from there, sometimes even cannulating the axillary vein itself (remember the vessel changes names as it crosses over the 1st rib).
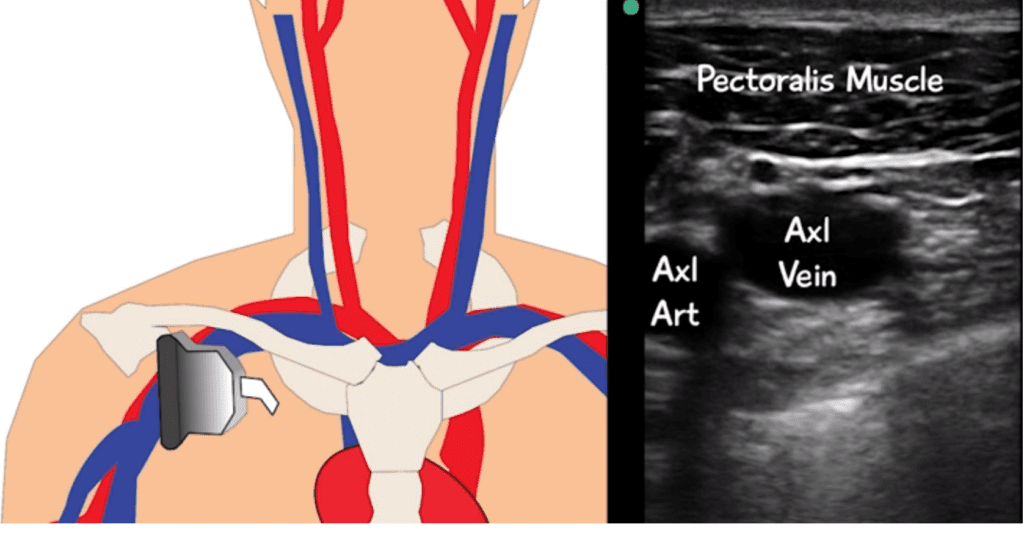
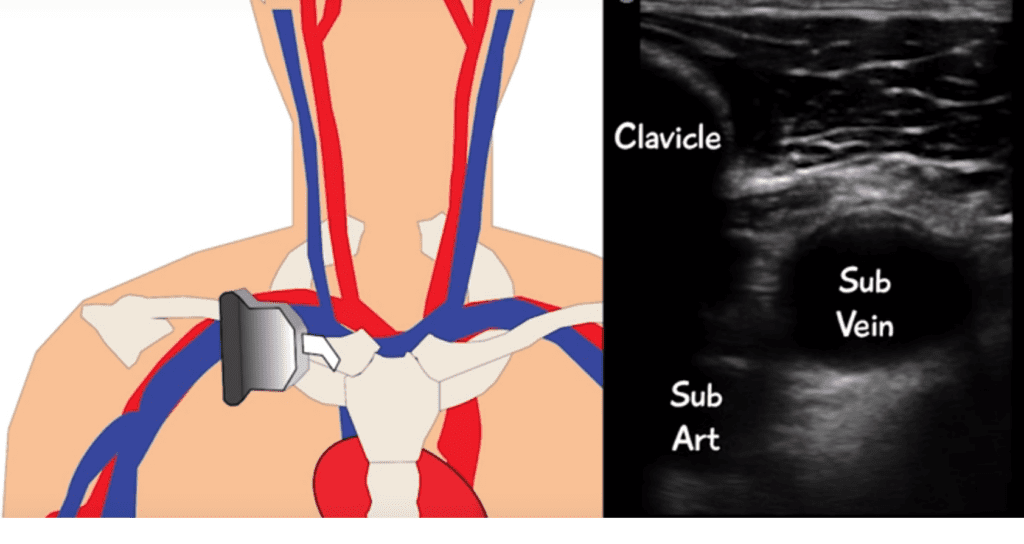
The axillary cannulation has the advantage of often being separated from the pleura more than the subclavian. It also has not yet begun to dive under the clavicle. If you are capable, a longitudinal approach is often recommended as an additional safeguard against pleura injury.
Here is a video of a subclavian CVC placed under US guidance in the longitudinal plane.
And to show you this is not just a handful of people who have this anatomy, here is my own axillary vein becoming the subclavian. It is pretty easy to spot where to cannulate the vein just before the clavicle comes into view.
Additional Moves
PART
For additional safety, Dr. Senussi et al recommend the Pleural Avoidance with Rib Trajectory (PART) technique. In doing this, the operator attempts to cannulate the subclavian vein (really the axillary vein) in a region that has a rib as a backstop. In their paper they discuss the use of the second rib for this purpose. This is definitely a pro move that requires a far bit of knowledge of anatomy and skill in ultrasound.
SHRUG technique from PULMCrit
With the shrug technique, a conscious patient shrugs their shoulders upward, pulling it up and out of the way of venous cannulation. This positioning can be replicated in the less-than-cooperative or unconscious patient by bracing the patient’s elbow upward for shrug position.
A Final Thought on Landmark Technique Subclavian
While blind subclavian lines are far from ideal, in a truly emergent situation they can be life saving. It is worth noting that an alterative to the traditional infraclavicular approach exists in the supraclavicular approach, or “pocket shot.” In this approach you are feeling the lateral head of the sternocleomastoid (SCM) muscle and its connection to the clavicle. Right at that connection point there is a soft indent into the neck, termed “the pocket.” After finding the pocket, you insert your needle 1 cm lateral to the SCM muscle and 1 cm posterior to the clavicle, aiming for the contralateral nipple. A 2020 Meta-analysis of eight RCTs found this approach to be superior to the blind infraclavicular approach.
For more on this approach, check out this review article.
Conclusions
1. The subclavian vein has been shown with a reasonable degree of quality evidence to have the lowest risks of infection and thrombosis.
2. Mechanical complications plague the placement of a subclavian line, which can be overcome by ultrasound.
3. The US guided subclavian is made easier by:
- Looking out toward the axillary vein for actual canulation
- Using a rib to protect against puncturing the pleura
- Having the patient shrug
4. If doing a blind subclavian, the supraclavicular approach may be better… in the right hands.
Keeping your skills sharp is an uphill battle. Let SimKit do the heavy lifting in your skill maintenance. Procedural training can and should be easy, done in your home or department, and work within your schedule. We want you to be confident and competent clinicians, and we have the tools to help.
References & Additional Readings
Mansfield PF1, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization.N Engl J Med. 1994 Dec 29;331(26):1735-8. [pubmed]
Gualtieri E, Deppe SA, Sipperly ME, Thompson DR. Subclavian venous catheterization: greater success rate for less experienced operators using ultrasound guidance. Crit Care Med. 1995 Apr;23(4):692-7. [pubmed]
Lefrant JY, Cuvillon P, Bénézet JF, Dauzat M, Peray P, Saïssi G, de La Coussaye JE, Eledjam JJ. Pulsed Doppler ultrasonography guidance for catheterization of the subclavian vein: a randomized study. Anesthesiology. 1998 May;88(5):1195-201. [pubmed]
Palepu GB, Deven J, Subrahmanyam M, Mohan S. Impact of ultrasonography on central venous catheter insertion in intensive care. Indian J Radiol Imaging. 2009 Jul-Sep;19(3):191-8. [pubmed]
Fragou M1, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, Karabinis A, Saranteas T, Poularas J, Papanikolaou J, Davlouros P, Labropoulos N, Karakitsos D. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011 Jul;39(7):1607-12. [pubmed]
Merrer J1, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, Rigaud JP, Casciani D, Misset B, Bosquet C, Outin H, Brun-Buisson C, Nitenberg G; French Catheter Study Group in Intensive Care. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001 Aug 8;286(6):700-7. [pubmed]
Shah A, Smith A, Panchatsharam S. Ultrasound-guided subclavian venous catheterisation – is this the way forward? A narrative review. Int J Clin Pract. 2013 Aug;67(8):726-32. [pubmed]
Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, Marqué S, Thuong M, Pottier V, Ramakers M, Savary B, Seguin A, Valette X, Terzi N, Sauneuf B, Cattoir V, Mermel LA, du Cheyron D; 3SITES Study Group. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015 Sep 24;373(13):1220-9. [pubmed]
Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015 Jan 9;1:CD011447. [pubmed]
Goetz AM1, Wagener MM, Miller JM, Muder RR. Risk of infection due to central venous catheters: effect of site of placement and catheter type. Infect Control Hosp Epidemiol. 1998 Nov;19(11):842-5. [pubmed]
Robinson JF, Robinson WA, Cohn A, Garg K, Armstrong JD, 2nd. Perforation of the great vessels during central venous line placement. Arch Intern Med 1995; 155:1225–8. [pubmed]
Senussi MH, Kantamneni PC, Omranian A, Latifi M, Hanane T, Mireles-Cabodevila E, Chaisson NF, Duggal A, Moghekar A. Revisiting Ultrasound-Guided Subclavian/Axillary Vein Cannulations: Importance of Pleural Avoidance With Rib Trajectory. J Intensive Care Med. 2017 Jul;32(6):396-399. [pubmed]
Chen Q, Long Q, Liang JQ, Tang TX, Yang B. Comparative evaluation of the clinical safety and efficiency of supraclavicular and infraclavicular approaches for subclavian venous catheterization in adults: A meta-analysis. The American Journal of Emergency Medicine 38.7 (2020): 1475-1480. [pubmed]


